Abstract
Research Article
Trends of Antibiotic Resistance among Uropathogens in Medical vs. Non-Medical Departments of Al-Shifa Medical Complex in Gaza Strip: A Retrospective, Cross-Sectional Study
Khaled Alkhodari*, Yasmin Al-Shurafa, Hammam AL-louh and Rafat Lubbad
Published: 12 January, 2024 | Volume 7 - Issue 1 | Pages: 001-005
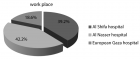
Antibiotic resistance is a growing global crisis, straining healthcare systems and leaving us with limited options to combat drug-resistant bacteria. This retrospective, cross-sectional study examines the prevalence of antibiotic resistance patterns among urinary tract infections (UTIs) in Al-Shifa Hospital’s medical departments in comparison with non-medical departments using data from microbiology laboratory archives over a one-year period.
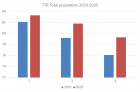
From the examined urine cultures about 25% were obtained from internal medicine departments and double the number was obtained from non-medical departments. The positive rate was around 35% and about two-thirds of the samples were collected from female patients.
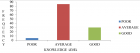
Among all departments, Enterobacteriaceae spp. were found to be the most frequently isolated uropathogens, accounting for 80% of cases. However, resistance rates varied depending on the specific organism and antibiotic used. For instance, E. coli showed a resistance rate of only 5% against meropenem, while amoxicillin-clavulanic acid exhibited a resistance rate exceeding 95%.
Importantly, the study revealed a significant disparity in resistance rates between medical and non-medical departments, specifically concerning third-generation cephalosporins. In internal medicine departments, resistance rates were alarmingly high, with cefotaxime, ceftriaxone, and ceftazidime showing resistance rates of 75%, 75% and 66.5% respectively. In contrast, non-medical departments displayed lower resistance rates, approximately 60%, 60% and 40%, respectively.
In summary, this research sheds light on the escalating problem of antibiotic resistance in UTIs and emphasizes the discrepancy in resistance rates between medical and non-medical departments. Urgent efforts are required to address this issue and find effective solutions to prevent the rise of untreatable bacterial infections.
Read Full Article HTML DOI: 10.29328/journal.ijcmbt.1001028 Cite this Article Read Full Article PDF
Keywords:
Anti-bacterial agents; Urinary tract infections; Antibiotic resistance; Uropathogens; Palestine; Gaza strip
References
- Wagenlehner FME, Bjerklund Johansen TE, Cai T, Koves B, Kranz J, Pilatz A, Tandogdu Z. Epidemiology, definition and treatment of complicated urinary tract infections. Nat Rev Urol. 2020 Oct;17(10):586-600. doi: 10.1038/s41585-020-0362-4. Epub 2020 Aug 25. PMID: 32843751.
- Foxman B. Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am. 2014 Mar;28(1):1-13. doi: 10.1016/j.idc.2013.09.003. Epub 2013 Dec 8. PMID: 24484571.
- Complicated urinary tract infections: developing drugs for treatment Revision 1. 2018. https://www.fda.gov/media/71313/download.
- Founou RC, Founou LL, Essack SY. Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS One. 2017 Dec 21;12(12):e0189621. doi: 10.1371/journal.pone.0189621. PMID: 29267306; PMCID: PMC5739407.
- Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health. 2015;109(7):309-18. doi: 10.1179/2047773215Y.0000000030. Epub 2015 Sep 7. PMID: 26343252; PMCID: PMC4768623.
- Llor C, Bjerrum L. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf. 2014 Dec;5(6):229-41. doi: 10.1177/2042098614554919. PMID: 25436105; PMCID: PMC4232501.
- Surveillance of Antimicrobial Resistance in Europe. 2017. https://www.ecdc.europa.eu/sites/default/files/documents/EARS-Net-report-2017-update-jan-2019.pdf.
- Antibiotic resistance threats in the United States; 2013. https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf.
- Dadgostar P. Antimicrobial Resistance: Implications and Costs. Infect Drug Resist. 2019 Dec 20;12:3903-3910. doi: 10.2147/IDR.S234610. PMID: 31908502; PMCID: PMC6929930.
- Klein EY, Van Boeckel TP, Martinez EM, Pant S, Gandra S, Levin SA, Goossens H, Laxminarayan R. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci U S A. 2018 Apr 10;115(15):E3463-E3470. doi: 10.1073/pnas.1717295115. Epub 2018 Mar 26. PMID: 29581252; PMCID: PMC5899442.
- Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015 Apr;40(4):277-83. PMID: 25859123; PMCID: PMC4378521.
- World Health Organization. Regional Office for South-East A: Guidelines on standard operating procedures for microbiology. WHO Regional Office for South-East Asia, New Delhi. 2000.
- Elmanama AA, Elaiwa NM, El-Ottol AE, Abu-Elamreen FH. Antibiotic resistance of uropathogens isolated from Al-Shifa hospital in Gaza Strip in 2002. J Chemother. 2006 Jun;18(3):298-302. doi: 10.1179/joc.2006.18.3.298. PMID: 17129841.
- Elmanama AA, El-Aydi I, Al-Reefi M, Ferwana N. Antibiogram of bacterial isolates from clinical specimens during 2018-2020 at Al-Aqsa hospital, Gaza, Palestine. The International Arabic Journal of Antimicrobial Agents. 2022; 12: 10;3823/867.
- Elmanama AA, Abu Tayyem NES, Sjölander I. Antimicrobial resistance of bacterial isolates from the clinical and hospital environment in Gaza Strip, Palestine: A review over 20-year. The International Arabic Journal of Antimicrobial Agents. 2021; 10.3823/859.
- Kot B. Antibiotic Resistance Among Uropathogenic Escherichia coli. Pol J Microbiol. 2019 Dec;68(4):403-415. doi: 10.33073/pjm-2019-048. Epub 2019 Dec 5. PMID: 31880885; PMCID: PMC7260639.
- Wang S, Zhao S, Zhou Y, Jin S, Ye T, Pan X. Antibiotic resistance spectrum of colistrains from different samples and age-grouped patients: a 10-year retrospective study. BMJ Open. 2023 Apr 12;13(4):e067490. doi: 10.1136/bmjopen-2022-067490. PMID: 37045577; PMCID: PMC10106033.
- Abdel Gawad AM, Ashry WMO, El-Ghannam S, Hussein M, Yousef A. Antibiotic resistance profile of common uropathogens during COVID-19 pandemic: hospital based epidemiologic study. BMC Microbiol. 2023 Jan 25;23(1):28. doi: 10.1186/s12866-023-02773-5. PMID: 36694128; PMCID: PMC9873538.
Figures:
Similar Articles
-
Hypochlorous acid has emerged as a potential alternative to conventional antibiotics due to its broad-spectrum antimicrobial activityMaher M Akl*. Hypochlorous acid has emerged as a potential alternative to conventional antibiotics due to its broad-spectrum antimicrobial activity. . 2023 doi: 10.29328/journal.ijcmbt.1001026; 6: 001-004
-
Trends of Antibiotic Resistance among Uropathogens in Medical vs. Non-Medical Departments of Al-Shifa Medical Complex in Gaza Strip: A Retrospective, Cross-Sectional StudyKhaled Alkhodari*, Yasmin Al-Shurafa, Hammam AL-louh, Rafat Lubbad. Trends of Antibiotic Resistance among Uropathogens in Medical vs. Non-Medical Departments of Al-Shifa Medical Complex in Gaza Strip: A Retrospective, Cross-Sectional Study. . 2024 doi: 10.29328/journal.ijcmbt.1001028; 7: 001-005
Recently Viewed
-
Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean sectionToon Wen Tang*,Phoon Wai Leng Jessie. Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean section. Clin J Obstet Gynecol. 2021: doi: 10.29328/journal.cjog.1001094; 4: 092-095
-
Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience ResearchAlex, Gideon S*,Olanrewaju Oluwaseun Oke,Joy Wilberforce Ekokojde,Tolulope Judah Gbayisomore,Martina C. Anene-Ogbe,Farounbi Glory,Joshua Ayodele Yusuf. Adult Neurogenesis: A Review of Current Perspectives and Implications for Neuroscience Research. J Neurosci Neurol Disord. 2024: doi: 10.29328/journal.jnnd.1001102; 8: 106-114
-
Late discover of a traumatic cardiac injury: Case reportBenlafqih C,Bouhdadi H*,Bakkali A,Rhissassi J,Sayah R,Laaroussi M. Late discover of a traumatic cardiac injury: Case report. J Cardiol Cardiovasc Med. 2019: doi: 10.29328/journal.jccm.1001048; 4: 100-102
-
A two-phase sonographic study among women with infertility who first had normal sonographic findingsKalu Ochie*,Abraham John C. A two-phase sonographic study among women with infertility who first had normal sonographic findings. Clin J Obstet Gynecol. 2022: doi: 10.29328/journal.cjog.1001117; 5: 101-103
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024: doi: 10.29328/journal.acr.1001099; 8: 075-077
Most Viewed
-
Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth EnhancersH Pérez-Aguilar*, M Lacruz-Asaro, F Arán-Ais. Evaluation of Biostimulants Based on Recovered Protein Hydrolysates from Animal By-products as Plant Growth Enhancers. J Plant Sci Phytopathol. 2023 doi: 10.29328/journal.jpsp.1001104; 7: 042-047
-
Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case PresentationJulian A Purrinos*, Ramzi Younis. Sinonasal Myxoma Extending into the Orbit in a 4-Year Old: A Case Presentation. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001099; 8: 075-077
-
Feasibility study of magnetic sensing for detecting single-neuron action potentialsDenis Tonini,Kai Wu,Renata Saha,Jian-Ping Wang*. Feasibility study of magnetic sensing for detecting single-neuron action potentials. Ann Biomed Sci Eng. 2022 doi: 10.29328/journal.abse.1001018; 6: 019-029
-
Pediatric Dysgerminoma: Unveiling a Rare Ovarian TumorFaten Limaiem*, Khalil Saffar, Ahmed Halouani. Pediatric Dysgerminoma: Unveiling a Rare Ovarian Tumor. Arch Case Rep. 2024 doi: 10.29328/journal.acr.1001087; 8: 010-013
-
Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative reviewKhashayar Maroufi*. Physical activity can change the physiological and psychological circumstances during COVID-19 pandemic: A narrative review. J Sports Med Ther. 2021 doi: 10.29328/journal.jsmt.1001051; 6: 001-007

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."